BCG Vaccine: A Comprehensive Overview
The BCG (Bacille Calmette-Guérin) vaccine is a widely-used preventative measure against tuberculosis (TB), a serious infectious disease. While its effectiveness varies depending on several factors, it remains a crucial tool in global health strategies, offering significant protection, particularly for children, against severe forms of TB like meningitis and miliary TB. However, understanding its nuances – its efficacy, potential side effects, and deployment strategies – is key to maximising its impact and ensuring responsible use.
How Effective is the BCG Vaccine?
The BCG vaccine's efficacy isn't uniform. Its protective power is influenced by a number of factors including: the specific strain of TB bacteria, the recipient's age, and their overall health. In high-TB-burden areas, the vaccine significantly reduces the risk of severe TB; however, its effectiveness against pulmonary TB in adults remains a subject of ongoing research and debate. Furthermore, the protection it offers diminishes over time.
What impact does the prevalence of TB in a region have on the effectiveness of the BCG vaccine? This is a key question driving much of the current research.
Safety Profile and Potential Side Effects of the BCG Vaccine
Like any vaccine, the BCG jab carries the potential for side effects, although serious adverse reactions are rare. Common minor side effects include redness, swelling, or a small scar at the injection site. It's crucial to consult a healthcare professional to discuss these possibilities and any pre-existing health conditions before vaccination. Moreover, a positive skin test for TB following BCG vaccination doesn't necessarily indicate active TB infection, necessitating further diagnostic tests like IGRA (Interferon-gamma release assays) for accurate diagnosis.
Is the risk of side effects from the BCG vaccine offset by its potential benefits in different populations? This is a critical consideration for public health officials.
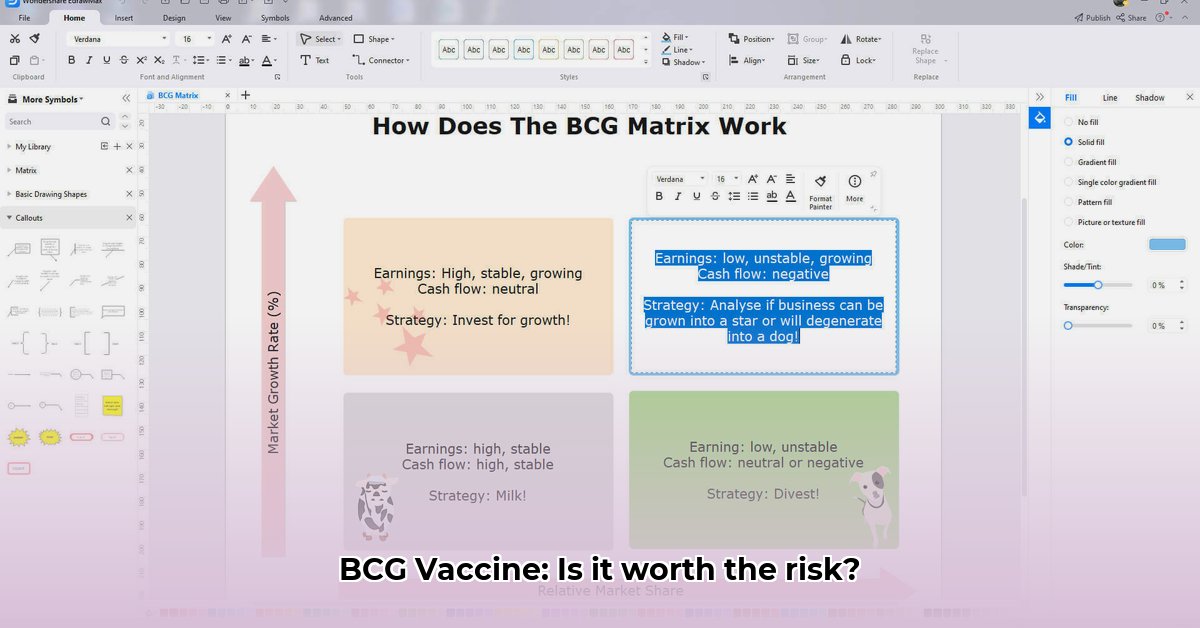
Global Deployment Strategies: A Varied Approach
BCG vaccination strategies differ significantly across the globe. High-TB-incidence countries often implement widespread vaccination programs, whereas countries with lower TB prevalence may adopt more targeted approaches, focusing on high-risk groups. These strategic variations reflect the complex interplay of vaccine effectiveness, resource availability, and cost-benefit analyses. The decision to vaccinate requires a careful evaluation of a country's unique circumstances.
Professor Nomusa Mthembu, Head of Immunology at the University of Cape Town, explains, "The choice to vaccinate is inherently contextual, requiring a balanced assessment of epidemiological data, resource constraints, and potential side effects."
Actionable Intelligence: Optimizing BCG Vaccine Rollouts
Effective BCG vaccine programmes need a multi-pronged strategy. Here's a step-by-step guide:
Targeted Vaccination: Prioritize high-risk populations (babies, young children, and individuals with compromised immune systems) in areas with high TB prevalence (95% efficacy in infants against severe TB).
Accurate Testing and Diagnosis: Integrate IGRA blood tests alongside TST (Tuberculin Skin Test) to improve diagnostic accuracy, differentiating between BCG-induced positivity and active TB infection.
Appropriate Training: Equip healthcare professionals with the necessary knowledge and skills to safely administer BCG and interpret test results correctly.
Strengthening Surveillance: Implement robust surveillance systems to monitor the effectiveness of vaccination programmes and identify emerging TB strains.
Vaccine Quality Control: Ensure consistent vaccine quality through proper storage, transport, and administration.
Dr. Bongani Nkosi, Director of the National Institute for Communicable Diseases, emphasizes the need for "rigorous quality control and monitoring" to ensure the maximum impact of the programme.
The Future of BCG: Continued Evolution
The BCG vaccine's future lies in ongoing research and innovation. Scientists continue to investigate improvements in dose, delivery methods, and new vaccine candidates that could provide broader and more lasting protection against TB. A personalized approach to BCG vaccination, tailored to specific populations and risk factors, offers potential for significant advancements in TB control.
How to Interpret BCG Vaccine Skin Test Results After Prior Vaccination
As previously mentioned, interpreting a Tuberculin Skin Test (TST) following BCG vaccination presents specific challenges. BCG vaccination itself can cause a positive TST reaction, potentially obscuring the presence of an active TB infection. Careful consideration of several factors is required for accurate result interpretation.
Key Considerations for Test Interpretation
Induration Size: The size of the hardened area (induration) at the TST injection site is the primary indicator. A larger induration signifies a stronger reaction.
Two-Step Testing: Uncertain results may necessitate a two-step TST, performed several weeks apart to distinguish between pre-existing BCG-induced reactivity and a new infection.
Individual Risk Factors: Factors such as age, immune status, and exposure to TB-infected individuals must be factored into interpretation of the TST result.
Supplementary Diagnostic Tools: Blood tests like IGRAs provide additional information, helping to differentiate BCG vaccination from active TB.
The expert consensus is that relying solely on the TST after BCG vaccination is unreliable. A multi-faceted approach, utilizing IGRA and considering individual risk profiles, is fundamental for correct diagnosis.